Hemorrhoid surgery is a medical procedure to remove swollen veins in your anus or rectum. Many people share the same question—is hemorrhoid surgery covered by insurance? Knowing the answer to it is important so you can prepare yourself before the procedure.
The cost of hemorrhoid surgery can vary depending on several factors like your healthcare institution and treatment. Although most hemorrhoid surgery procedures are covered by insurance, you may have to pay out-of-pocket for additional services.
What Is Hemorrhoid?
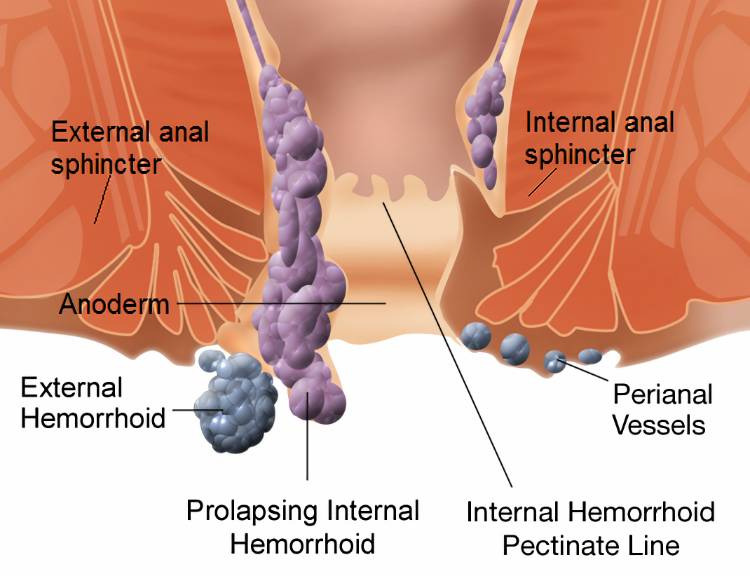
Hemorrhoids are enlarged veins inside or outside your rectum. They can cause rectal bleeding, pain, discomfort, and anal itching. Symptomatic hemorrhoids are quite common and the risk becomes greater if you are pregnant, have obesity, and have a low-fiber diet.
Hemorrhoids are less likely to pose serious health issues, even some of them can be cured with home treatment. You can relieve the symptoms by applying OTC medication, drinking enough water, and increasing your fiber intake.
But if your symptoms do not increase or get worse and disturb your daily activities, visit your nearby healthcare provider to get help. Your doctor may suggest rubber band ligation or surgeries depending on the severity. Is hemorrhoid surgery covered by insurance? Keep scrolling for the answer.
Does Insurance Cover Hemorrhoid Surgery?
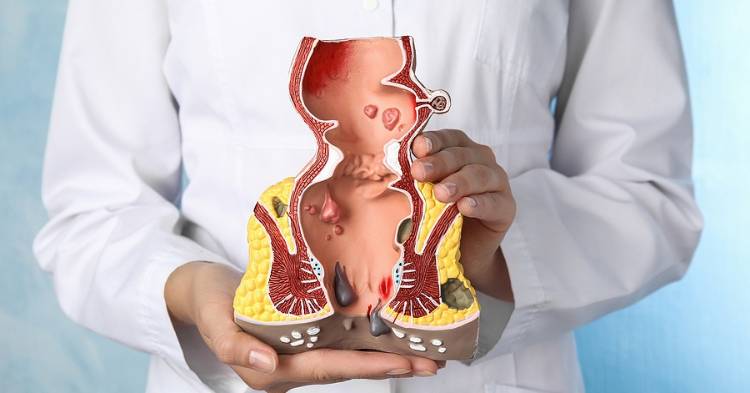
There are various treatments to get rid of hemorrhoids these days, including surgical and non-surgical procedures. Your healthcare provider will suggest the best treatment based on your condition and severity level.
Diverse treatment options for hemorrhoid influences the cost the patient must pay. For example, hemorrhoidectomy which is known as a traditional method to remove hemorrhoids costs $9,500 on average. Meanwhile, hemorrhoid ligation that involves less invasive surgery costs $1,500 on average.
Is hemorrhoid surgery covered by insurance? Yes, a majority of health insurance plans cover symptomatic hemorrhoid treatments including surgery. Depending on your insurance plan, you may need to pay a lower out-of-pocket cost than the average price.
Medicare can cover the hemorrhoid surgery cost in a public hospital for eligible residents. On the other hand, a private health insurance holder can get partial coverage and you still have to pay out-of-pocket for the rest.
Also Read:
- Is Laser Therapy Covered by Insurance?
- Does Insurance Cover Dentaa Bonding? Explained
- Permanent Health Insurance: All You Need to Know
How to Minimize Your Cost

Now you know your health insurance plan may not fully cover the treatment cost. For this reason, it is important to learn how to minimize the cost so it does not collapse your finance.
Choose Your Hospital
If you choose a private hospital for the treatment, you can minimize the cost by choosing a hospital and healthcare provider that have an agreement with your insurer. Also, find information about how much the insurance covers for your treatment.
Ask Your GP for Referral
Before visiting a specialist, you will need to consult your general practitioner (GP). If you want to minimize the cost for whatever reason, ask your GP to find a qualified specialist with minimum expenses who is still competent to perform the treatment.
Ask Your Specialist
Is hemorrhoid surgery covered by insurance? Yes, but you may have to pay for the gap out-of-pocket. Another way to minimize the cost of hemorrhoid surgery is to ask your specialist, especially if you already have one.
Ask them if you have a full cover agreement from your insurer. You may also ask what hospitals have full coverage with your health insurance.
Types of Hemorrhoid Surgery

Type of surgical treatment is another contributing factor for out-of-pocket costs you have to pay, considering the cost of these procedures may vary. Here are various surgical treatments to remove hemorrhoids.
Rubber Band Ligation
Band ligation or banding is a less invasive procedure. The doctor places a small rubber band around the base of your hemorrhoids to stop the blood supply to the vein. It is ideally used to treat up to grade 3 internal hemorrhoids.
Hemorrhoidectomy
Suitable for grades 3-4 with prolapsed internal and large external hemorrhoids, this procedure is performed under anesthesia. After the hemorrhoids are removed, you may feel pain that lasts about 1 week.
Hemorrhoidopexy
Also known as stapling, this procedure requires either general or regional anesthesia. It fixes prolapsed hemorrhoids into place and stops the blood tissue. Hemorrhoidopexy is often suggested for grades 3-4.
Is hemorrhoid surgery covered by insurance? Yes, most health insurance plans cover hemorrhoid surgery. Depending on several factors like your insurer, healthcare facility, and type of surgery, you may have to pay out-of-pocket after the procedure.







